《鄉民大學問EP.37》字幕版|台南政治版圖有變數?謝龍介有機會?黃偉哲全說了!台南市長前哨戰開打!陳亭妃、王定宇、林俊憲鴨子划水 邱明玉揭他勝算高!黃智賢轉綠?被哥哥盜帳號?黃偉哲霸氣回應現場笑翻!
NOW影音
更多NOW影音焦點
更多焦點-

TPASS將滿周年!抽「乘車金」最高15000元 澎湖有望5月上路
TPASS 月票自去年7月1日上路啟用迄今,已實施10個月,交通部今(24)日宣布感恩回饋抽獎活動開跑,抽「乘車金」最高15000元。公路局指出,目前全台剩下金馬澎尚未加入,澎湖規劃兩種方式,預計最快
2024-04-24 13:04
-

金價要轉空了嗎?短線急殺一度失守2300美元 專家喊:還沒有
國際金價在衝上2431美元新高後,短線出現急殺,一度下探2291美元,跌了140美元,市場也關注金價是否要轉空了?對此,外匯專家李其展今(24)日接受《NOWnews今日新聞》採訪時表示,這確實是近來
2024-04-24 12:54
-

一粒姊姊甜蜜官宣男友宋嘉翔!現身樂天2軍球場 戀情早有跡可循
台鋼雄鷹啦啦隊成員「一粒」因「葉保弟應援曲」的魔性舞步爆紅,連帶仙氣十足的雙胞胎姊姊Joy也跟著爆紅。今(23)日,Joy也在IG上甜蜜公開球員男友,是樂天桃猿潛力「大物」捕手宋嘉翔。事實上,Joy早
2024-04-23 16:58
-

母親節團聚夢碎!彰化99歲前鄉長夫人命喪火場 生前曾急喊兒名
彰化縣埤頭鄉堤頭路一處三合院民宅,今(24)日凌晨4時許發生火警,造成屋內99歲陳姓阿嬤因逃生不及喪命。據悉,死者為已故前鄉長陳全的妻子,平時與子孫同住一個屋簷下,屋主二兒子表示,火災當下聽見老母親不
2024-04-24 13:15
精選專題
要聞
更多要聞-

美提供19億美元軍援 邱國正:提供那些裝備或服務都可以去談
美國眾議院日前通過「2024 年印度太平洋安全補充撥款法案」,並將送入參議院審查,法案中19億美元(約600億台幣),指定供美國防部用於協助台灣及區域夥伴國家。國防部長邱國正今(24)日表示,美方既然
2024-04-24 12:49
-

強震重創花蓮經濟!黃暐瀚:傅崐萁赴中國爭取陸客來台 才有生機
國民黨立院黨團總召傅崐萁在立院開議期間訪問中國,引發爭議,雖然連黨內都認為不宜,不過傅崐萁可能僅會微調時間,但訪中勢在必行。資深媒體人黃暐瀚說,0403強震重創花蓮,傅崐萁趕著赴中,就是指望陸客來台,
2024-04-24 12:32
-

傅崐萁不甩黨內異音堅持赴中 綠委曝「藍營OS」:真的像病毒一樣
花蓮餘震不斷,至今已逾千起,不過國民黨立院黨團總召傅崐萁25日將率約10位立委訪問北京,行程仍照舊不改,不僅被民進黨批評,就連國民黨內也雜音不斷。民進黨立委吳思瑤今(24)日受訪時表示,昨天有看到國民
2024-04-24 12:18
-

監委為35年前舊案約詢 侯友宜喊「坦蕩蕩」:檢視過去非製造對立
新北市長侯友宜近期收到監察院約詢通知,監委高涌誠與林郁容要調查35年前「世台會總幹事羅益世闖關回台遭驅逐出境案」,並命侯友宜今天到監院接受調查,挨轟「政治追殺」。侯友宜一早抵達監察院,經過約1.5小時
2024-04-24 12:17
新奇
更多新奇-

別管60元便當了!全聯「買1水果」送保鮮盒 優惠瘋傳:錯過等1年
先別管60元便當了!全聯福利中心因為經常推出許多新品,或者是期間限定的產品,因此婆媽常常會在臉書社團上討論分享。然而近日就有不少人分享去全聯購買「寶石紅奇異果」,並且開箱分享口感,沒想到卻釣出內行婆媽
2024-04-24 11:57
-

王彩樺是「台灣諧音始祖」!12年前神講解爆紅 觀眾挖出影片服她
相信有不少人之都知道台灣人真的非常愛用諧音,不過是餐廳、手搖飲甚至是健身房的名字,都能利用諧音來取名,像是知名連鎖飲料店「可不可(渴不渴)」、「鶴茶樓(喝茶嘍)」都是諧音。然而,近日就有網友挖出國民岳
2024-04-24 10:53
-

《池水抽光好吃驚》來台灣!抽光中興湖 驚見「激似鯊魚」外來種
日本知名綜藝節目《池水抽光好吃驚》在今年3月份來台灣,由主持人田村淳與興大生組成多達1百人的「池水台日隊」,抽光國立中興大學內的「中興湖」池水,結果捕撈出近3百隻生物,裡面甚至還有「激似鯊魚」的外來種
2024-04-23 18:07
-
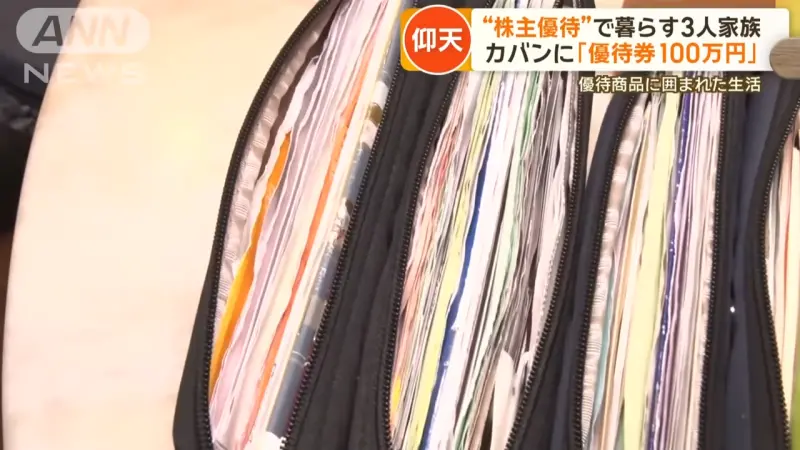
7年買710支股票不賣!1家3口靠「股東福利」活超爽:出門不用花錢
台灣進入股東大會旺季,各家公司開始發放股東會紀念品,例如六福(2705)會發放價值1199元門票給6萬名股東,中鋼(2002)則送出超實用的抗菌多功能不鏽鋼砧板組,總是引發廣大討論。而在日本,更有奇人
2024-04-23 16:56
娛樂
更多娛樂-

小S大女兒是學霸!Elly錄取「這兩間頂尖名校」 媽不捨陪同赴美
綜藝天后小S(徐熙娣)結婚18年育有3名女兒,近日傳出18歲長女Elly(許曦文)將赴美攻讀名校南加大或加州大學,為名符其實的學霸,對此,媽媽小S證實此事,透露很替Elly開心,卻又不捨女兒到國外讀書
2024-04-24 12:40
-

許美靜開唱挨轟偷懶!伍佰、五月天「互動歌迷」反激起演唱會高潮
新加坡歌手「小王菲」許美靜唱紅〈城裡的月光〉、〈遺憾〉、〈蔓延〉等曲,日前在南京舉辦復出演唱會,被踢爆2個多小時的演出、只唱30分鐘,引發歌迷怒吼:「退票!」同樣喜歡在演唱會上「互動歌迷」的伍佰、五月
2024-04-24 12:07
-

小嫻不孕被問「為何不收養」 她無奈:公婆怎會要沒血緣的孩子?
小嫻(黃瑜嫻)14歲發現自己月經沒有來,檢查後被證實天生沒有子宮,右側卵巢也因為有良性畸胎瘤而切除,終身無法生育,她月初赴立法院參加「《人工生殖法》條文修正草案公聽會」,昨(23)日為自己及不孕女性發
2024-04-24 11:55
-

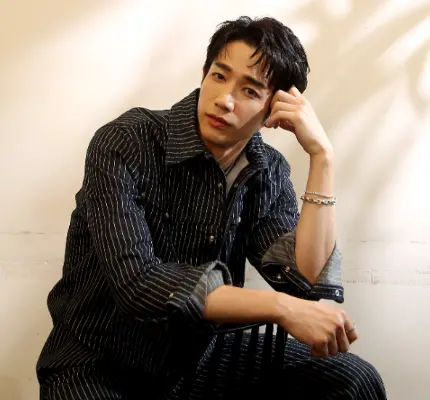
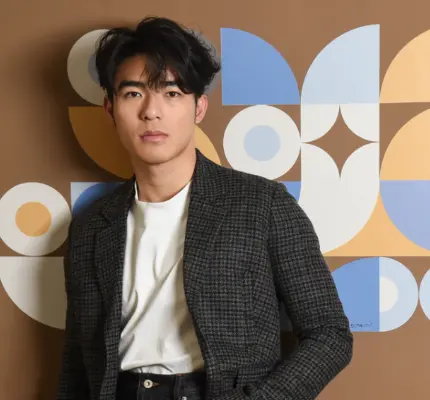
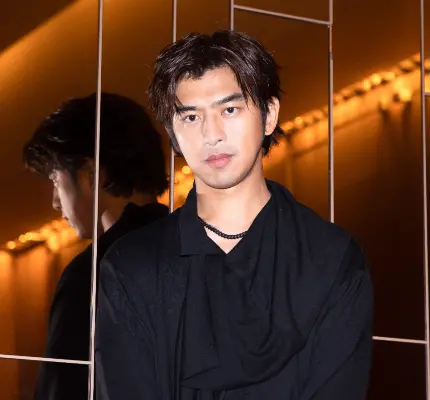
蕭閎仁哭「國家警報沒存到我號碼」被轟沒常識 本人:4月都沒響
花蓮外海4月3日發生規模7.2強震,半個月過去,大小餘震仍不斷發生,近日還出現6級以上震度,創作歌手蕭閎仁昨(23)日發文不解地問,為何自己沒有收到國家警報簡訊,有網友控訴提醒蕭閎仁要達4級才會被示警
2024-04-24 11:08
運動
更多運動-

NBA季後賽/太陽系列賽吞2連敗!Kevin Durant:還不是放棄的時候
NBA鳳凰城太陽今(24)日季後賽首輪G2,以93:105不敵明尼蘇達灰狼,太陽在系列賽大比分以0勝、2敗落後,雖太陽目前處於劣勢,但陣中球星Kevin Durant與Devin Booker在賽後記
2024-04-24 12:33
-

Jokic「大哥」與球迷爆發口角!還毆打湖人迷 聯盟決定介入調查
NBA美國職籃季後賽,在昨(23)日G2由洛杉磯湖人交手丹佛金塊,金塊靠著當家主控Jamal Murray中距離絕殺,以101:99絕殺湖人在系列賽大比分拿下2勝、0敗,雖金塊在這場贏下比賽,但卻在昨
2024-04-24 12:17
-

大谷翔平「閃電」轟炸裂!主帥羅伯茲也嚇到 道奇4:1擊敗國民
大谷翔平又開轟!洛杉磯道奇隊今(24)日作客國民隊主場,日籍二刀流好手大谷翔平,轟出右外野全壘打,這是他生涯第177轟,本季第6轟,大谷不但轟出本季最遠全壘打,這發全壘打初速高達191公里,幫助道奇以
2024-04-24 12:05
-

NBA季後賽/Pascal Siakam轟37分!溜馬125:108公鹿 還創一紀錄
NBA季後賽密爾瓦基公鹿今(24)日季後賽首輪G2在主場交手印第安納溜馬,此戰公鹿主力「字母哥」Giannis Antetokounmpo依舊因傷高掛免戰牌,由Damian Lillard單核帶隊,雙
2024-04-24 11:15
財經生活
更多財經生活-

快訊/雨勢升級擴大!13縣市「豪雨特報」 苗栗時雨量逼近60毫米
今(24)日受鋒面影響,全台各地整天皆有降雨機率,中央氣象署發布「豪雨特報」,提醒民眾,鋒面影響易有短延時強降雨,苗栗更是出現59.5毫米的時雨量,務必注意雷擊及強陣風,且近期地震頻繁,山區土石鬆軟,
2024-04-24 13:15
-
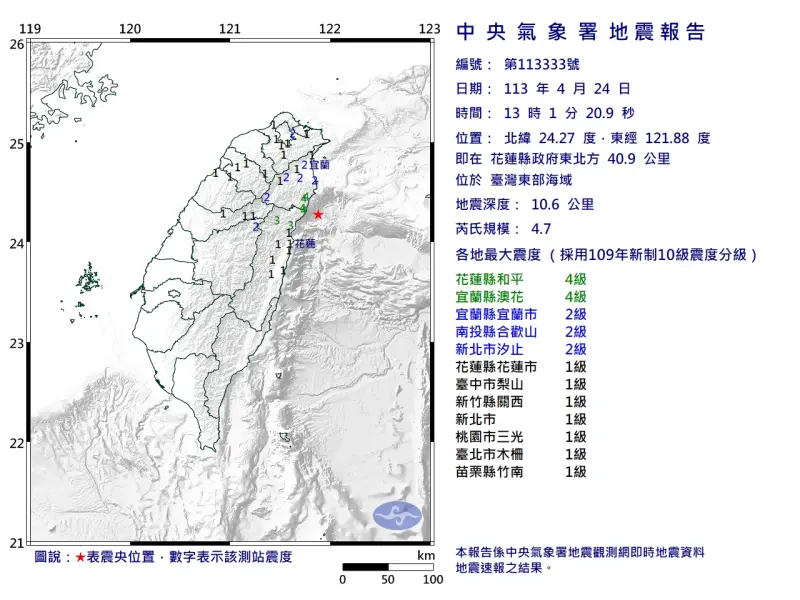
快訊/13:01「4.7極淺層地震」!花蓮最大震度4級 雙北也有感
中央氣象署地震測報中心表示,今(24)日下午1時01分台灣東部外海又發生芮氏規模4.7地震,震央位於花蓮縣政府東北方40.9公里 ,深度10.6公里屬於「極淺層地震」,測得最大震度在花蓮和宜蘭4級,其
2024-04-24 13:11
-

水庫救星快來!鋒面發威「石門水庫仍亮紅燈」 全台即時水情一覽
每年梅雨季前台灣會進入一波枯水期,上週石門水庫、寶山水庫、石岡壩、霧社水庫、仁義潭水庫等都亮起水情提醒,好消息是今(24)日起會有兩波鋒面接續襲台,為各地帶來高降雨機率,經過一早上的大雨特報,石門水庫
2024-04-24 12:32
-

水庫解渴就看這波!氣象署揭「豪雨轟炸」時間點 一週天氣一次看
全台水庫鬧水荒,急需降雨好好解渴,中央氣象署預報員徐仲毅指出,未來一週台灣天氣持續受鋒面影響較不穩定,明(25)日新一波鋒面接近,並在週五至週日(4/26至4/28)於台灣上空滯留徘徊,特別要留意週五
2024-04-24 12:12
全球
更多全球-

抗美援俄聯盟?北韓高官代表團罕見出訪伊朗 深化軍事合作掀關注
北韓對外經濟相尹正浩昨(23)日自平壤啟程前往伊朗,北韓官媒《朝中社》並未介紹此次行程的詳情與計畫,但這是北韓睽違5年再有高級官員出訪伊朗,時機恰逢伊朗與以色列緊張升溫之際,讓外界猜測北韓是否要與伊朗
2024-04-24 12:30
-
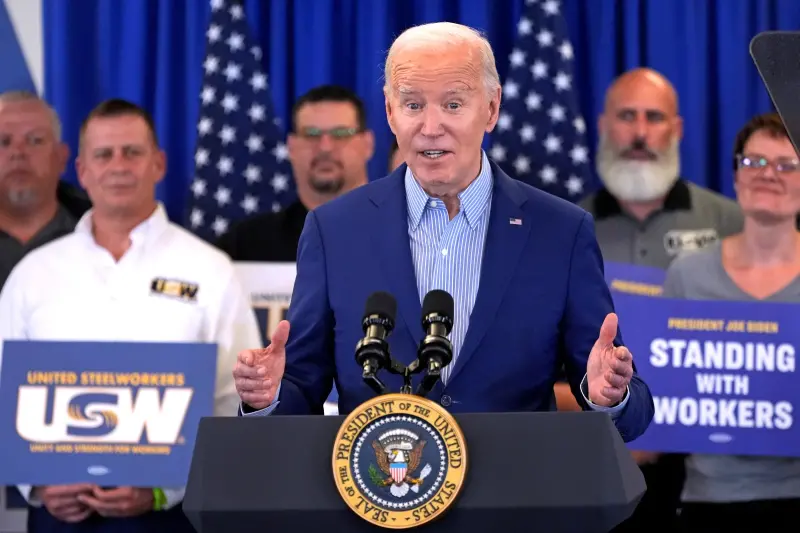
成功過關!美參院通過援以烏台法案 拜登迫不及待週三簽署
美國聯邦參議院23日以79票支持、18票反對,通過援助以色列、烏克蘭、台灣的包裹法案,該法案周三將上呈至拜登簽署。根據CNN報導,有15名共和黨人和3名民主黨人投下反對票,就在參議院通過後,美國聯邦參
2024-04-24 11:38
-

批美韓軍演是地區緊張禍首!金與正嗆:北韓將建立壓倒性軍事力量
北韓日前進行了首次核反擊演習,本月也曾發射測試大型彈頭的戰略巡弋飛彈,警告意味濃厚。而北韓領導人金正恩的胞妹金與正,今(24)日再度發表談話譴責美國和韓國頻繁聯合軍演,導致地區緊張局勢升級,揚言北韓將
2024-04-24 11:27
-

憲法法庭首次死刑存廢言詞辯論!全球還有多少國家保留死刑?
憲法法庭23日首次召開死刑存廢言詞辯論,掀起許多關注,司法院的直播更讓數千名網友觀看並討論。正反雙方針對死刑是否具嚇阻力等議題數次交鋒。死刑議題在各國皆有激烈討論,究竟還有哪些國家保有死刑,從近年的報
2024-04-24 10:49